Why Animal Research Matters
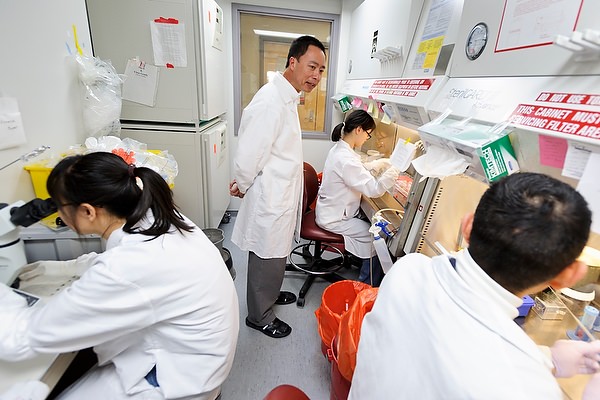
Animal research is an indispensable tool for understanding complex living organisms, and many University of Wisconsin–Madison research programs study animals as models of human disease and to explore basic biological processes. The university’s commitment to responsible and ethical research conducted under the attention of skilled veterinarians continues a long history of improving human and animal health and well-being.
News
How disabling one gene protects mice against Type 1 diabetes
UW–Madison researchers have discovered a mechanism that could one day help people at risk of developing the metabolic disease.
December 17, 2025A year of resilience and discovery
Despite uncertainty over federal funding, the university’s scientific community continued to advance knowledge and improve lives. Find out how from our favorite UW research stories of 2025.
December 15, 2025Congressional staff see UW–Madison research, federal investments up close
Congressional staff visited campus to see firsthand how national investments fuel discovery, improve lives, and strengthen Wisconsin’s economy.
November 25, 2025UW researchers turn to the tiny copepod for a big discovery, showing that gene location influences natural selection
The new study provides the first empirical evidence connecting the chromosomal location of genes to natural selection and how populations adapt to rapid environmental change.
November 21, 2025UW researchers tackle diabetes from multiple angles
Researchers at the UW School of Medicine and Public Health are working on new and improved treatments for diabetes and its complications. They’re also searching for what doesn’t yet exist: a cure.
November 18, 2025A new kidney — free of daily meds
Thanks to a cutting-edge clinical trial at UW–Madison, transplant patients are returning to a healthy life without anti-rejection drugs.
July 21, 2025- More animal research posts
- More UW News posts
Cell transplant treats Parkinson’s in mice under control of designer drug
A University of Wisconsin–Madison neuroscientist has inserted a genetic switch into nerve cells so a patient can alter their activity by taking designer drugs that would not affect any other cell. The cells in question are neurons and make the neurotransmitter dopamine, whose deficiency is the culprit in the widespread movement disorder Parkinson’s disease.